Pierro Lab
Neonatal Intestinal Disorders Requiring Surgery
The primary focus of our research is on searching for novel treatment strategies for Necrotizing Enterocolitis (NEC) in the animal model and to translate this to humans. We have established in vitro and in vivo experimental studies using techniques and models established in our laboratory. In vitro, we utilize intestinal epithelial cells or intestinal organoids; in vivo we use neonatal models of NEC in mice.
Recent News!
APPY Trial – The Lancet 2025
The prestigious medical journal, The Lancet, has just published a large study (APPY trial) designed by the publication‘s senior author, Dr. Agostino Pierro.
To conduct this landmark study, Dr. Pierro established an international collaborative network of experts across 14 centers in 6 countries and 3 continents. The APPY Trial – Appendicectomy versus antibiotics for acute uncomplicated appendicitis, is the first large-scale, randomized controlled trial to compare these two treatment options in children.
The trial ran between January 2016 and December 2021and included 936 children, aged 5 to 16 years with suspected non-perforated appendicitis. Participants in this study were assigned to either receive antibiotics or undergo surgery (appendicectomy).
The APPY Trial concluded that antibiotic treatment for uncomplicated appendicitis in children was inferior to appendicectomy.
This Trial outcome provides critical evidence to guide future treatment guidelines. The study fills a knowledge gap in appendicitis treatment and provides evidence-based talking points for discussing treatment options with parents.
Dr. Pierro and his team will continue exploring the most effective treatment strategies for children with appendicitis.
Interested in joining our lab?
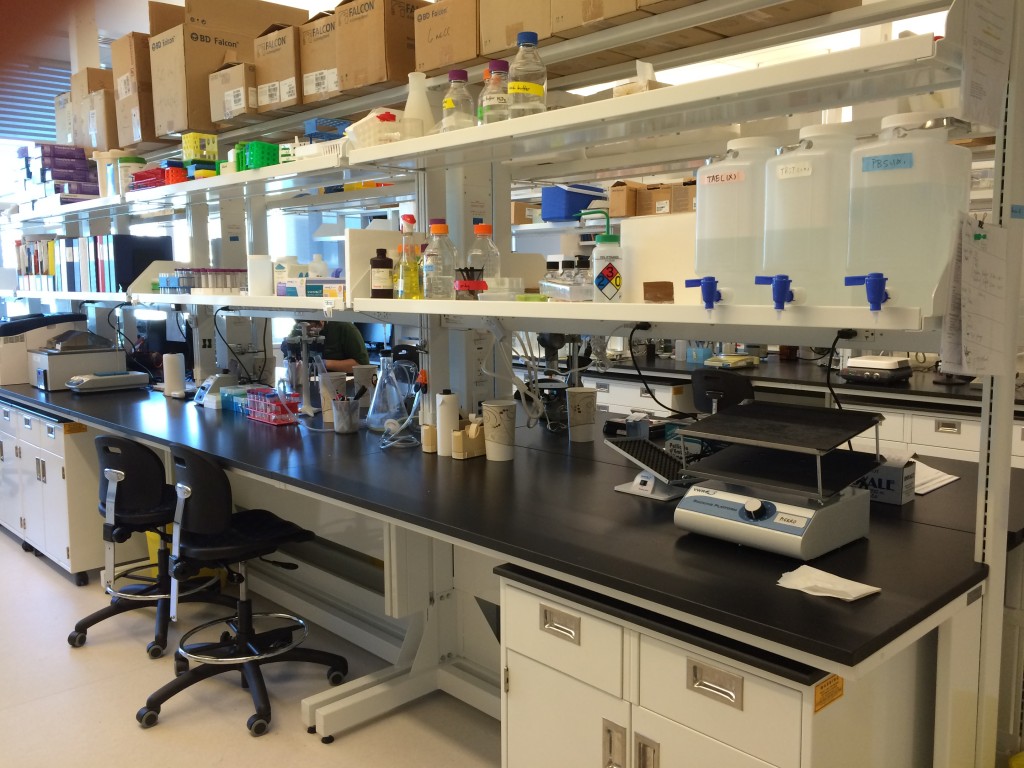
Lab bench in the Pierro lab on the 10th floor of the PGCRL
The Pierro lab is located at the SickKids Research Institute in downtown Toronto, Ontario, Canada. SickKids is the most research-intensive hospital in Canada, dedicated to improving child health. Within the Research Institute, there is great focus on training, with many positions for graduate students, postdoctoral fellows, research fellows and summer students.
We are looking for potential graduate students (MSc and PhD). Please contact Paul Fellows or Carol Lee, with an attached CV.
