Interested in following our research? Join our Lunch & Learn mailing list!
Current Studies
Stepped-Care Online Parent Support following Congenital Heart Disease: A Randomized Control Trial
- PI: Dr. Tricia Williams
- Partially funded by the Canadian Institutes of Health Research (CIHR)
This is a single-site, two-arm, single-blinded randomized clinical trial designed to assess 1) the efficacy of I-InTERACT-North in improving positive parenting skills and child behaviour in families of children with congenital heart disease (CHD), and 2) the feasibility and acceptability of the program.
What’s involved?
- Families will complete a set of baseline questionnaires. They will be randomized to receive I-InTERACT-North therapy or care as usual (CAU) for a period of 12 months, after which they will be offered I-InTERACT-North. In both conditions, families will complete a set of questionnaires after 3 months, 6 months, and 12 months.
Interested in participating?
Families can participate in this study if they:
- Have a child 3-9 years old with congenital heart disease (CHD) who is a patient at The Hospital for Sick Children (SickKids)
- Live in Ontario
- Have concerns about their child’s behaviour and/or parent stress
For more information, please email: neuro.outcomes@sickkids.ca
Examining a virtual mental health stepped care approach to addressing needs of at-risk children and families
- PI: Dr. Tricia Williams
- Funded by the Canadian Institutes of Health Research (CIHR), Edwin Leong Centre for Healthy Children, Garry Hurvitz Centre for Brain and Mental Health
This study will evaluate the implementation of a stepped-care virtual parenting program (I-InTERACT-North) while observing and gathering information on the impact of the intervention (e.g., child behaviour and family well-being) for families of children with neurological conditions (e.g., stroke, preterm birth, epilepsy) or neurodevelopmental disorders (e.g., ADHD, ASD). We will gradually expand I-InTERACT-North eligibility to various clinics at The Hospital for Sick Children based on needs and previous research.
What’s involved?
- Families will be asked to complete a set of questionnaires at baseline. They will meet with a therapist (PhD student in clinical psychology or a licensed psychologist) to complete a consultation session, and may be invited to complete either the abbreviated or full version of I-InTERACT-North.
Interested in participating?
Families can participate in this study if they:
- Have a child between 3-9 years old who is a patient at The Hospital for Sick Children (SickKids)
- Live in Ontario
- Have concerns about their child’s behaviour and/or are interested in learning strategies to guide their child’s behaviour and restore positive feelings to their relationship
For more information, please email: neuro.outcomes@sickkids.ca
Past Studies
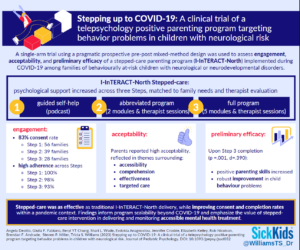
Stepping up to COVID-19: Examining a virtual mental health stepped care approach to addressing needs of at-risk children and families
- PI: Dr. Tricia Williams & Dr. Evdokia Anagnostou
- Funded by the Canadian Institutes of Health Research (CIHR)
This study evaluated a stepped-care model of an evidenced-based virtual mental health parent intervention (I-InTERACT-North; PI: Williams) with a strong record of success in virtual service delivery predating COVID-19. Stepped care models offer effective treatment and tailor treatment intensity and level of therapist involvement to families’ needs. For this study, I-InTERACT-North partnered with the Province of Ontario Neurodevelopmental Disorders (POND) Network (Co-PI: Anagnostou), a large, well-characterized diverse cohort of children and youth across Ontario with neurodevelopmental conditions.
We found that positive parenting skills increased among parents who completed the abbreviated or full version of I-InTERACT-North. Child behaviour concerns decreased among families who completed the full program. Parents also reported high acceptability of the program, describing it as accessible, easy to understand, and effective. Read the full publication by Dr. Angela Deotto and colleagues here: https://doi.org/10.1093%2Fjpepsy%2Fjsad032
Surviving and thriving: A feasibility trial of an eHealth parent-child intervention targeting common mental health outcomes following neonatal brain injury
- PI: Dr. Tricia Williams
- Partially funded by the Centre for Brain and Mental Health and Edwin S.H Leong Centre for Healthy Centre
We are currently completing a pre-post pilot feasibility trial of the 7-session I-InTERACT parenting program at The Hospital for Sick Children (SickKids) among families following medical illness/brain injury and most recently were awarded COVID-19 specific funding to extend the study to include other families in Neurology, Psychology and Psychiatry at SickKids and Holland Bloorview Kids Rehabilitation hospital.
Associated Publications
- Williams, T. S., Burek, B., Deotto, A., Ford, M. K., Green, R., & Wade, S. L. (2022). Pandemic Perils and Promise: Implementation of a Virtual Parenting Intervention during COVID-19 among Children with Early Neurological Conditions. Developmental Neurorehabilitation, 1-13. DOI: https://doi.org/10.1080/17518423.2022.2099996.
- Ford, M. K., Roberts, S. D., Andrade, B. F., Desrocher, M., Wade, S. L., Kohut, S. A., & Williams, T. S. (2022). Building I-INTERACT-North: Participatory Action Research Design of an Online Transdiagnostic Parent–Child Interaction Therapy Program to Optimize Congenital and Neurodevelopmental Risk. Journal of Clinical Psychology in Medical Settings, 1-12. DOI: https://doi.org/10.1007/s10880-022-09875-8.
- Burek, B., Ford, M.K., Hooper, M., Green, R., Kohut, S. A., Andrade, B., Ravi, M., Sananes, R., Desrocher, M., Miller, S., Wade, S.L., & Williams, T.S. (2020). Transdiagnostic feasibility trial of internet-based parenting intervention to reduce child behavioural difficulties associated with congenital and neonatal neurodevelopmental risk: Introducing I-InTERACT-North. The Clinical Neuropsychologist. 35 (5) 1030-1052. DOI: 10.1080/13854046.2020.1829071.
Parenting Experiences following Different Types of Neonatal Brain Injury: A pilot descriptive study
- PI: Dr. Tricia Williams
In the Parent Experience (PE) study, we used a patient-oriented research framework to examine parenting stress, coping, and mental health following their child’s diagnosis of neonatal brain injury or associated medical condition. Within the same study, we also conducted a mental health service needs assessment for these families. In the initial stages of this work, clinicians, researchers and parents created the primary study measures (the Parent Experiences Questionnaire).1 Parents of children diagnosed with a neonatal stroke, hypoxic ischemic encephalopathy (HIE) and congenital heart disease (CHD) participated in the study.
There were several key scholarly outcomes from this work, including 7 publications1-7, and several symposium talks and poster presentations advocating to reduce barriers to mental health services for families and to improve access to services that promote resilience in neonatal brain injury. Findings from the PE study emphasized the many parent-reported barriers to traditional mental health services, their strong interest in understanding how their child’s medical condition affects behaviour, and a pressing need to develop skills to better support their children’s socio-emotional development. Parents voiced a clear preference for individual, easily accessible eHealth initiatives over in-person and group therapies. Further, 100% of parents wanted a program to help them understand their child’s medical condition, with this need not met in existing general parent support programs. We also identified the relationship among parent mental health, child neurodevelopment, and coping strategies from this study.
The Parent Experiences Study has set the foundation for new initiatives that prioritize 1:1 eHealth initiatives that empower parent skill development and help parents understand the impact of their child’s medical history.
Associated publications
- Williams, T.S., McDonald, K.P., Roberts, S.D., Westmacott, R., Ahola Kohut, S., & Miller, S. (2018). In their own words: Building the parent experience questionnaire (PEQ) through participatory design. Brain Injury, 32(11), 1386-1396. DOI: 10.1080/02699052.2018.1495844
- Williams, T. S., McDonald, K. P., Roberts, S. D., Westmacott, R., Dlamini, N., & Tam, E. W. Y. (2019). Understanding early childhood resilience following neonatal brain injury from parents’ perspectives using a mixed-method design. JINS, 25(4), 390-402. DOI: 10.1017/S1355617719000079
- Williams, T. S., McDonald, K. P., Roberts, S. D., Chau, V., Seed, M., Miller, S. P., & Sananes, R. (2019). From diagnoses to ongoing journey: Parent experiences following congenital heart disease diagnoses. Journal of Pediatric Psychology, 44(8), 924-936. DOI: 10.1093/jpepsy/jsz055
- McDonald, K.P., Connolly, J., Roberts, S.D., Ford, M., Westmacott, R., Dlamini, N., Tam, E., & Williams, T.S. (2020). The response to stress questionnaire for parents following neonatal brain injury. Journal of Pediatric Psychology, 45(9), 1005-1015. DOI: 10.1093/jpepsy/jsaa059
- Peterson, R.K., Williams, T.S., Dlamini, N., & Westmacott, R. (2020). Parent experiences and developmental outcomes following neonatal stroke. The Clinical Neuropsychologist, published online. DOI: 10.1080/13854046.2020.1815855
- Danguecan, A., El Shahed, A.I., Somerset, E., Chun-Po, S.F., Ly, L.G., & Williams, T. (2020). Towards a biopsychosocial understanding of neurodevelopmental outcomes in children with hypoxic-ischemic encephalopathy: A mixed-methods study. The Clinical Neuropsychologist, published online. DOI: 10.1080/13854046.2020.1833987
- Shruti S. Vyas, Meghan K. Ford, Emily W. Y. Tam, Robyn Westmacott, Renee Sananes, Ranit Beck & Tricia S. Williams (2021). Intervention experiences among children with congenital and neonatal conditions impacting brain development: patterns of service utilization, barriers and future directions. The Clinical Neuropsychologist, published online. DOI: 10.1080/13854046.2020.1871516
- Roberts, S.D., Kazazian, V., Ford, M.K., Marini, D., Miller, S.P., Chau, V., Seed, M., Ly, L.G., Williams, T.S., & Sananes, R. (revise & resubmit). The association between parent stress, coping and mental health, and neurodevelopmental outcomes of infants with congenital heart disease. The Clinical Neuropsychologist (TCN), Special Edition.
Establishing a Retrospective Clinical Research Database for Patients with Congenital Heart Disease Undergoing Routine Clinical Neuropsychological Evaluation
- PI: Dr. Renee Sananes
Disruptions in Adolescent Brain Maturation Following Neonatal Stroke and the Impact of Intellectual Ability and Executive Function
- PI: Dr. Robyn Westmacott
Comprehensive Characterization of Social-Behavioural Phenotypes of NFT1
- PI: Dr. Katia Sinopoli
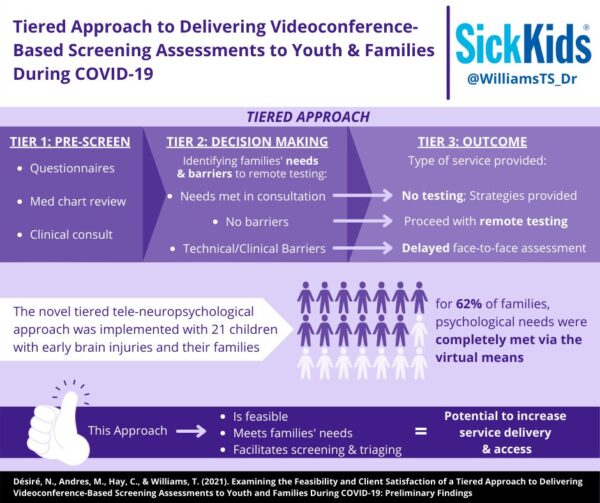
Examining the Feasibility and Client Satisfaction of a Tiered Approach to Delivering Videoconference-Based Screening Assessments to Youth and Families During COVID-19 and Beyond
- PI: Dr. Naddley Désiré
The current pandemic calls for consideration of innovative teleneuropsychological practices in providing complementary service delivery options to traditional in-person assessments. In response to this crisis, we examined the feasibility and client satisfaction of a novel tiered teleneuropsychological approach to provide informed and time-conscious direction to patients and families based on needs identified in the screening assessment. This novel approach consisted of a three-part assessment process which included:
- completion of online psychosocial questionnaires;
- an intake interview with a neuropsychologist via the hospital’s integrated secured Zoom platform; and
- completion of remote neuropsychological testing when eligible.
Preliminary findings of implementing this approach to meet families’ neuropsychological needs during COVID at SickKids Neonatal Neurology program are described and suggest that 62% of patients and families’ needs were completely met by virtual means. Results also indicate that this tiered approach to providing clinical care is feasible, facilitates efficient screening and triaging, and meets families’ needs while providing appropriate parent consultation. Globally, this novel tiered approach has the potential to increase service delivery to families, particularly in contexts where physical distancing regulations persist or where access to specialized tertiary pediatric hospital services is limited.