The vision of Ted Rogers Centre for Heart Research (TRCHR) is to transform and dramatically improve the future of heart health for children, adults and families across Canada and around the world. In the the centre aims to reduce hospitalization by 50 per cent and implement devices in patient homes to enable remote monitoring for cardiac function.
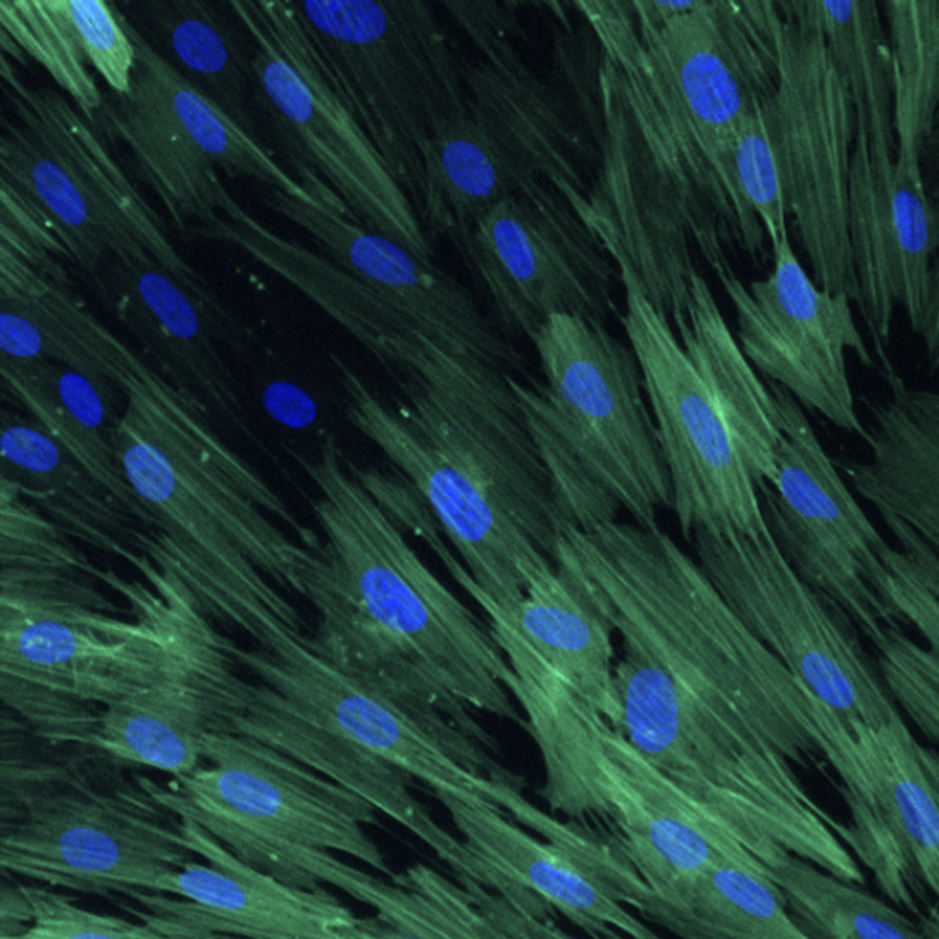
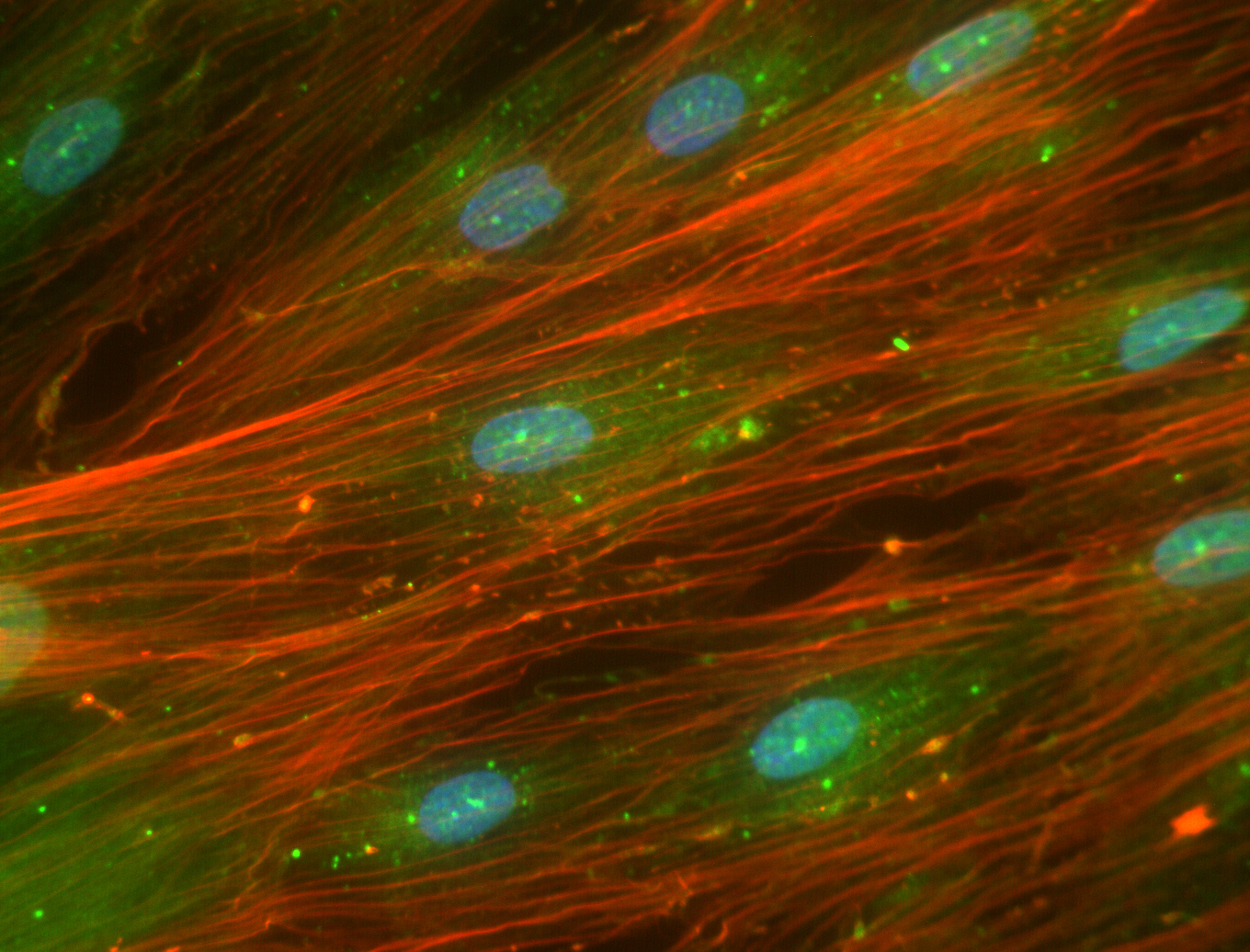
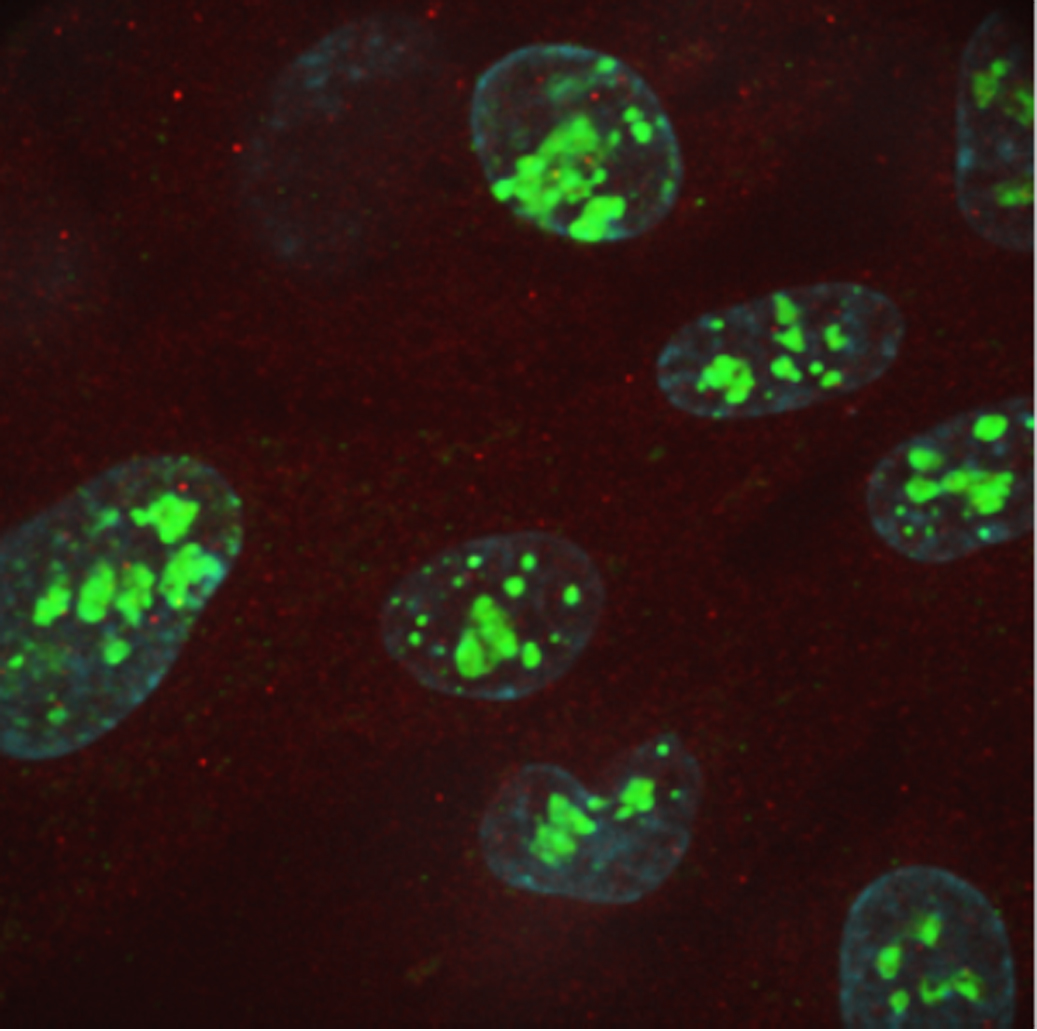
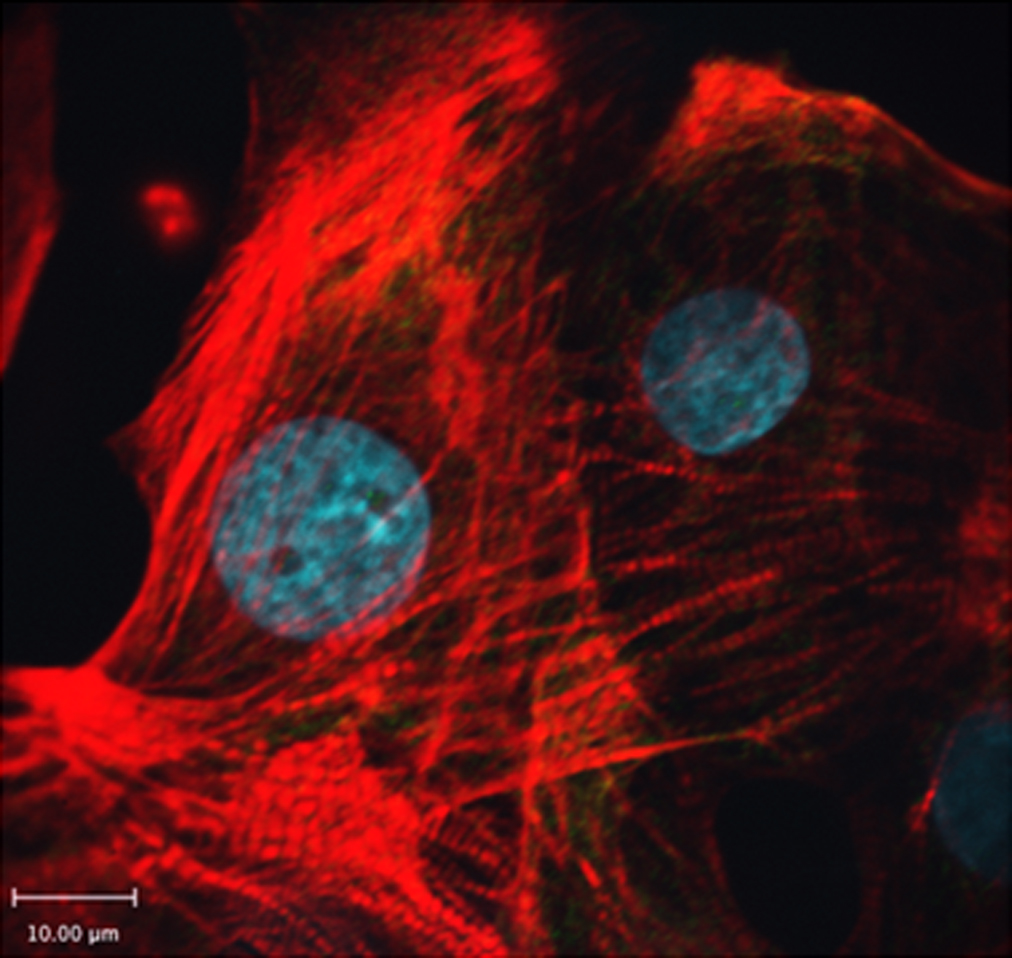
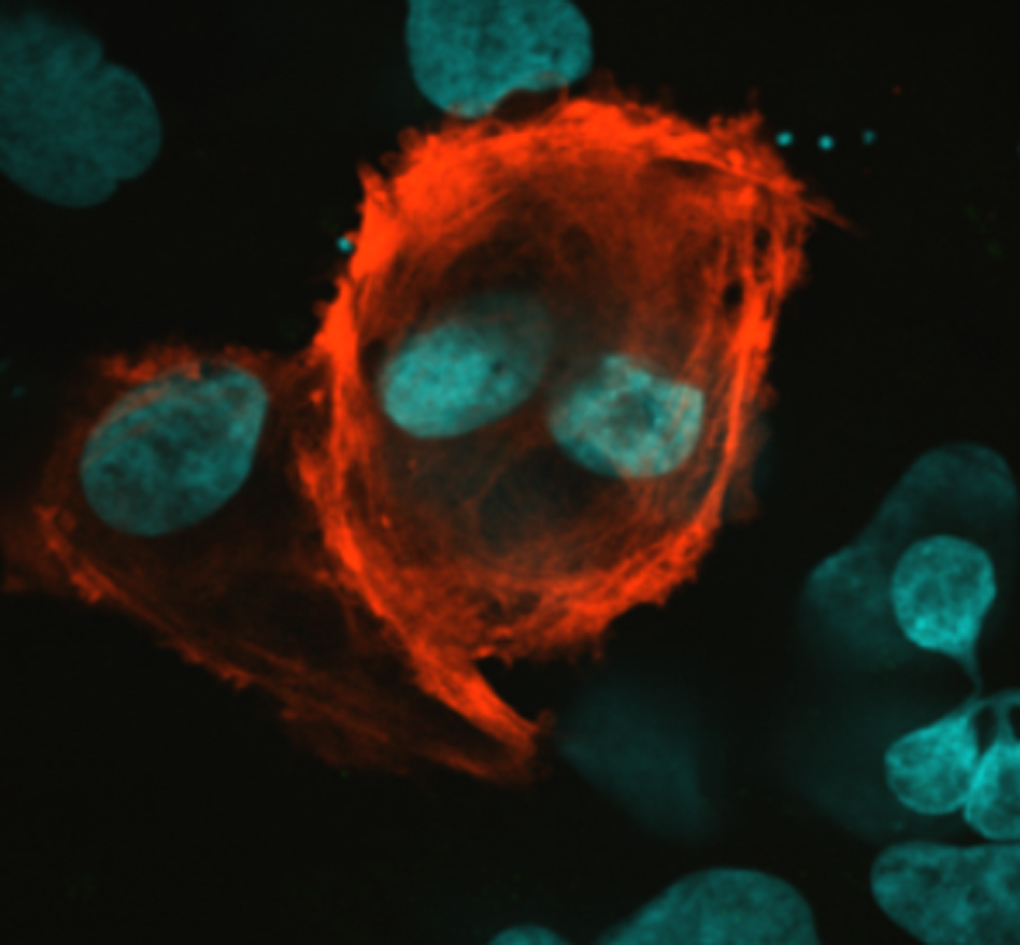
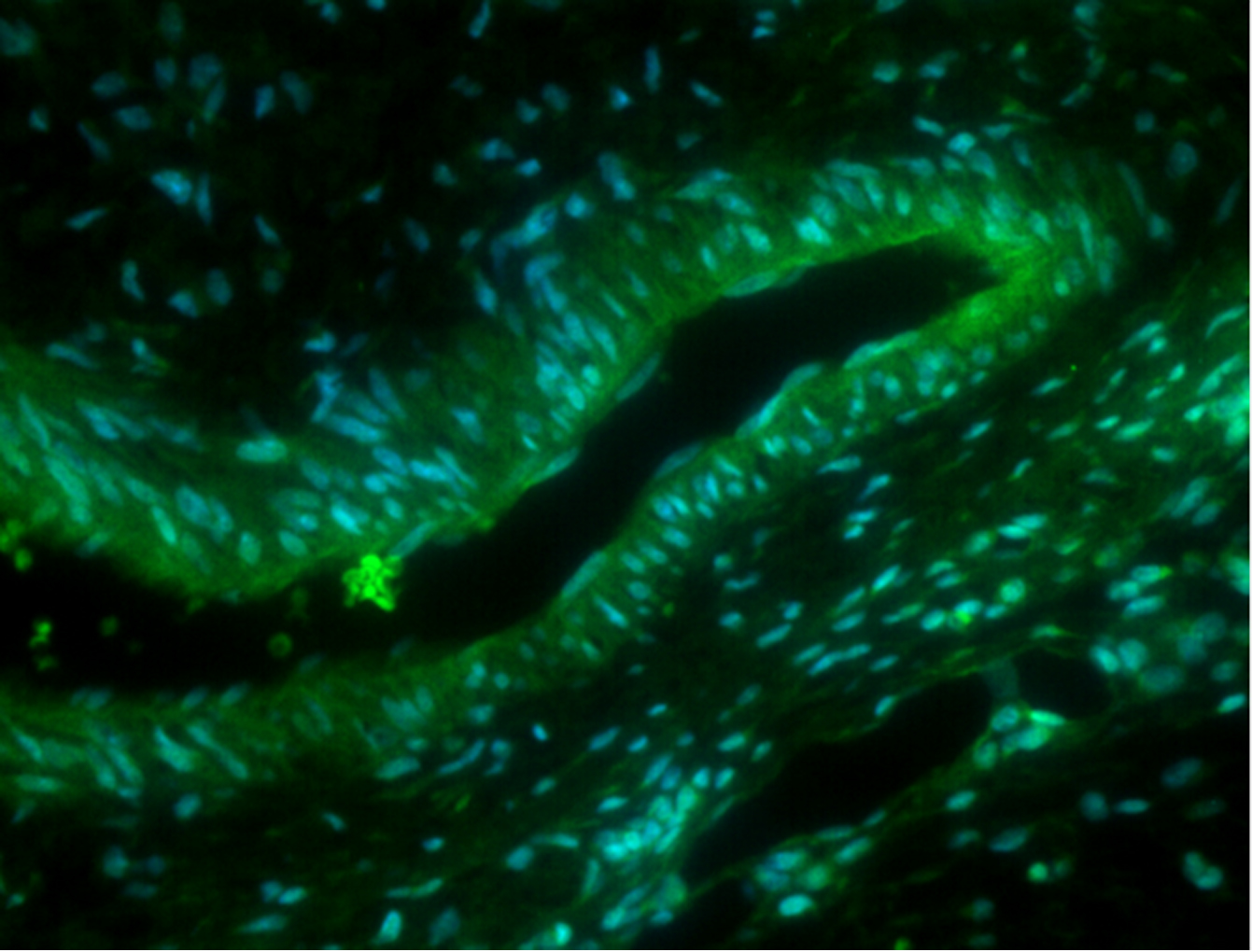
Our research team focuses on studying the genetics of heart diseases and we are constantly working on studies that aim to decode genetic foundation for cardiac diseases and to discover methods for implementing patient specific drugs to treat heart diseases. Currently our research team is also conducting myocardial tissue studies to decode the genetic foundations of cardiac disease on genomic, transcriptional, and translational levels. In these tissues proteomic studies are being done in parallel with RNA-sequencing to unravel biomarkers that play important roles in causing heart diseases and use that knowledge to aid us in searching for therapeutic targets.