The purpose of our research is to discover novel methods to prevent and treat intestinal injury in humans and enhance the quality-of-life and health of Canadians
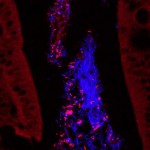
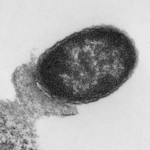
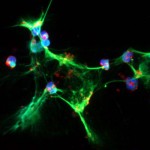
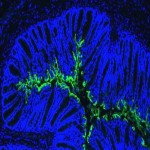
Inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS) describe a wide range of digestive disorders characterized by inflammation of the gastrointestinal tract, abdominal pain and diarrhea, which can be caused by a variety of factors including host genetics and infections with pathogenic bacteria. Our laboratory strives to better understand host-microbe interactions in the gut in the setting of disease. We investigate the mechanisms by which intestinal pathogens, such as enterohemorrhagic Escherichia coli and adherent-invasive E. coli from patients with Crohn’s disease affect epithelial cell models and relevant animal models of disease. Our research has led to the discovery of various treatment strategies (probiotics, prebiotics, and micronutrients) which alleviate or prevent disease outcome. We are well-known for our work with probiotics and have been fortunate to see our findings progress to prospective, randomized clinical trials.