Inspiration
The birth of a child is a truly extraordinary event. But not all children are born healthy. Approximately 1 in 10 children are born too early, and many children suffer brain injury in the perinatal period. These early life events predispose children to lifelong disability. Long term neurodevelopmental morbidity remains one of the greatest challenges for preterm and critically ill term infants. The protection and rehabilitation of the newborn brain is a final frontier in neonatology and is the focus of our work in the Kalish Lab. Moreover, there is growing recognition that exposures during early life program long term health risks, including neuropsychiatric disease. But the molecular mechanisms by which fetal and neonatal adversity shape neurodevelopment are poorly understood. We seek to address this major gap in knowledge by leveraging mouse models, human tissue, and advanced genomics to discover novel therapies in newborn brain injury, plasticity, and rehabilitation.
Brain development before birth
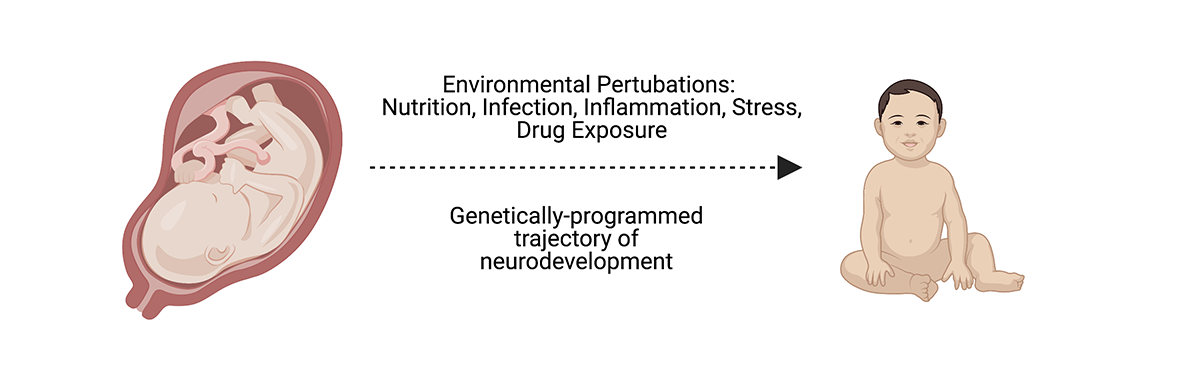
Fetal brain development is regulated by intrinsic genetic programs and extrinsic environmental signals, which converge to drive early neural circuit wiring. A multitude of intrauterine stressors, including malnutrition, infection, metabolic imbalance, and drug exposure, can disrupt the trajectory of early neurodevelopment, thereby predisposing offspring to profound, lifelong consequences for cognition and psychiatric disease risk. But how do these exposures impact neurodevelopment, and can these effects be reversed? We seek to understand intrauterine development in order to develop new therapies to shield the fetal brain from injury.
Placental regulation of brain development
The placenta is a hub of maternal-fetal crosstalk, and there is growing appreciation that perturbations in the maternal environment are conveyed to the fetus by changes in placental function. Placental dysfunction, resulting in intrauterine growth restriction and preeclampsia, result in serious illness to the mother and child. These conditions affect approximately 10% of pregnant women and contribute to maternal and childhood morbidity.
Neonatal neuroprotection
Perinatal brain injury, including hypoxic-ischemic encephalopathy, is a leading cause of newborn death and disability worldwide. We seek to explore molecular mechanisms underlying newborn brain injury, then identify therapeutic opportunities to intervene to mitigate neurologic injury. We are exploring a variety of interventions in pre-clinical and clinical settings to protect the newborn brain from injury.
Maternal brain plasticity
The female brain exhibits extraordinary plasticity during and after pregnancy. This adaptation is critical to maternal behavior and offspring wellbeing. However, the factors that regulate this reproductive plasticity are poorly understood. We are investigating pregnancy-associated changes that impact maternal behavior and the subsequent risk of post-partum neurospsychiatric disease.