The Rutka lab at The Hospital for Sick Children (SickKids) is led by world-renowned neurosurgeon Dr. James Rutka. Our goal is to bring hope to families and patients impacted by brain cancer, by finding effective treatments that improve patients’ quality of life and advance the field of brain tumour research.
The Rutka Lab
Advancing the field of brain tumour research.
The Rutka Lab
Advancing the field of brain
tumour research.
The Rutka Lab
Advancing the field of brain
tumour research.
“Everything is theoretically impossible, until it is done.”
– Robert A. Heinlein
Our Mission
Brain tumours are one of the most common types of tumours to occur in children and teens with close to 5,000 children being diagnosed in Canada each year. Our goal at the Rutka Lab is to:
- Bring hope to families and patients impacted by brain cancer
- Find effective treatments
- Improve patients’ quality of life
- Advance the field of paediatric brain cancer research
What Do We Study?
At the Rutka Lab we are working hard to better understand some of the most common childhood brain tumours: glioblastoma, medulloblastoma and diffuse intrinsic pontine glioma (DIPG).
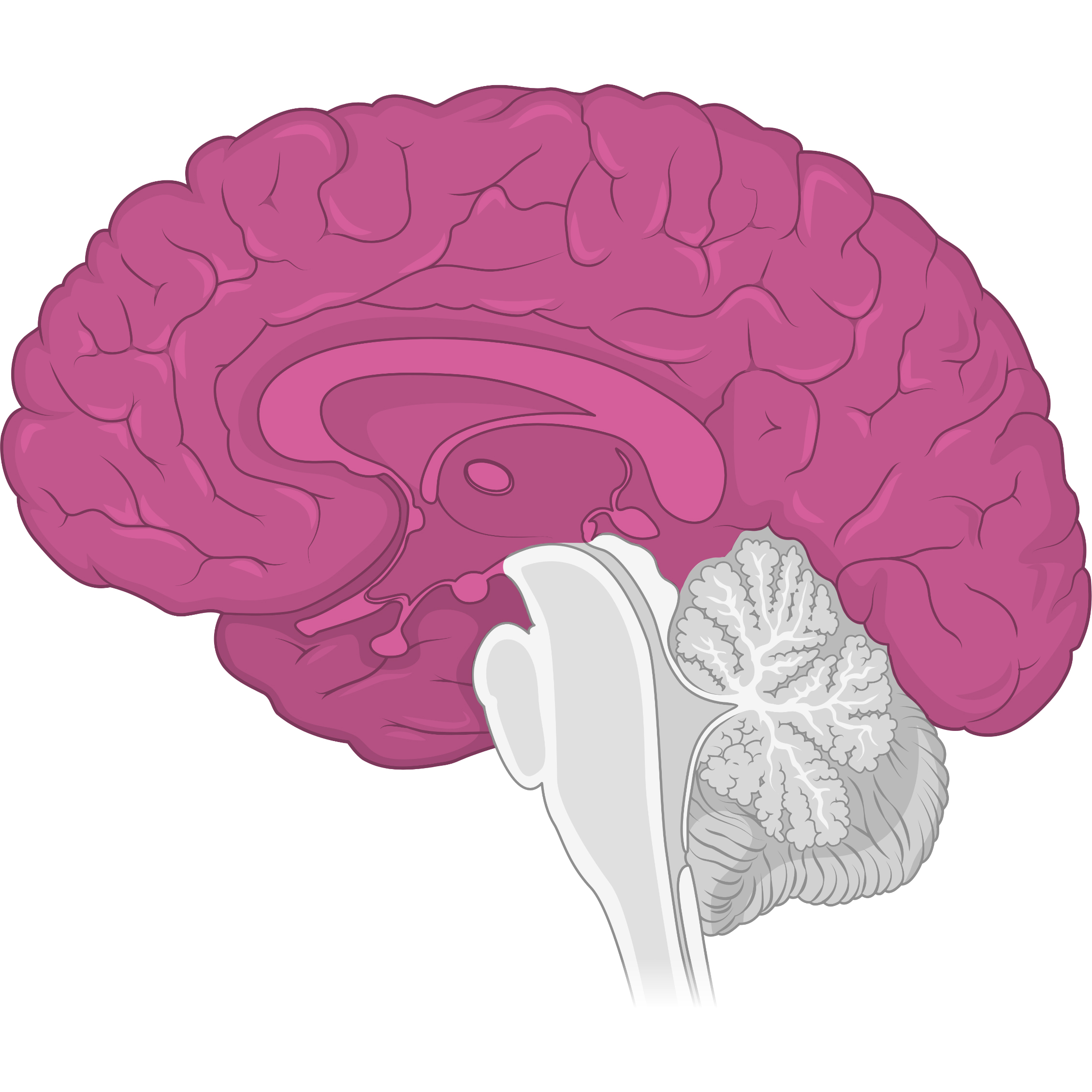
Glioblastoma
4 in every 100,000 people in Canada will be diagnosed with a glioblastoma. These tumours are highly aggressive and typically found in the cerebrum, the largest part of the brain.
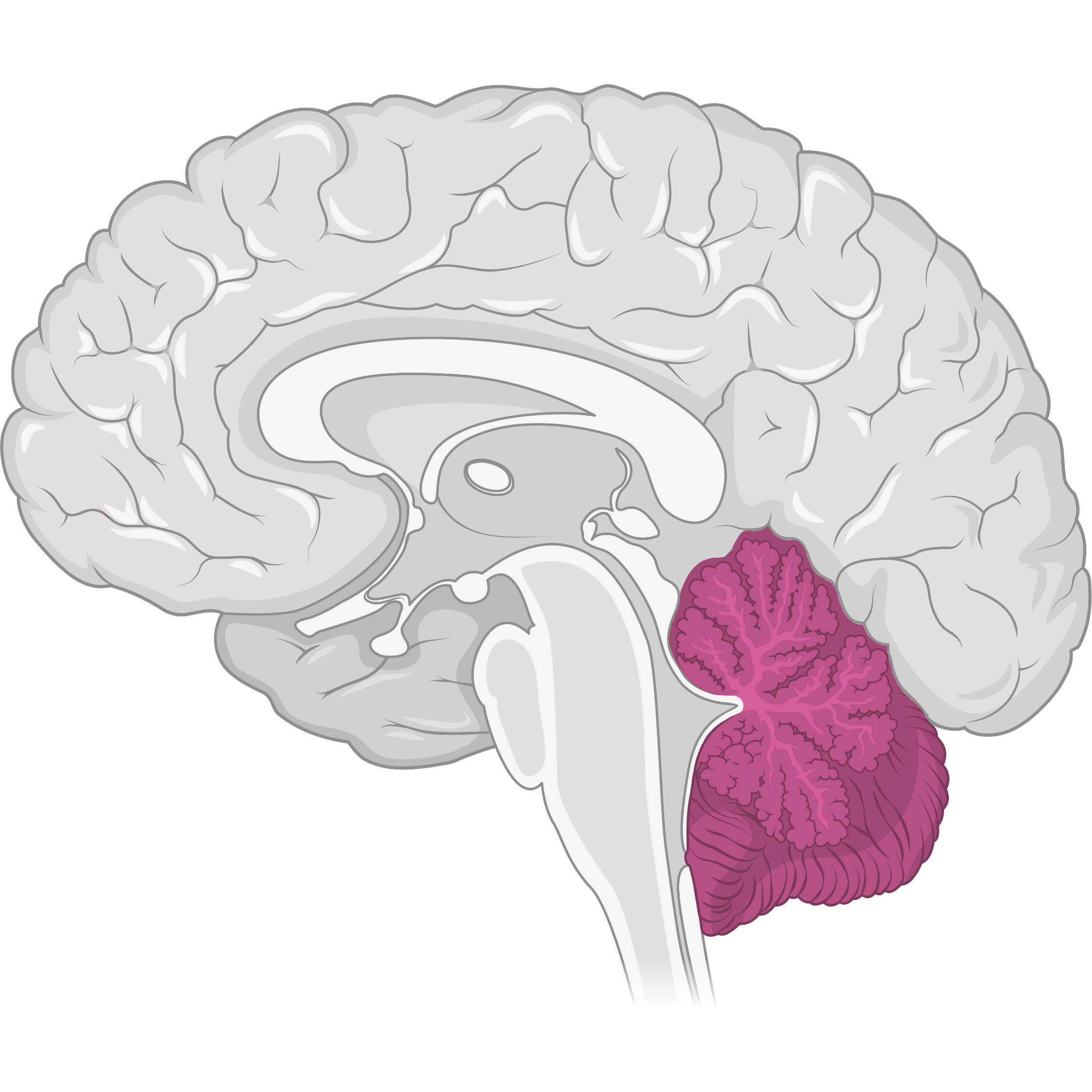
Medulloblastoma
40-50 children are diagnosed each year in Canada. Medulloblastomas are fast-growing tumours that are typically found in the cerebellum, which controls balance and coordination.
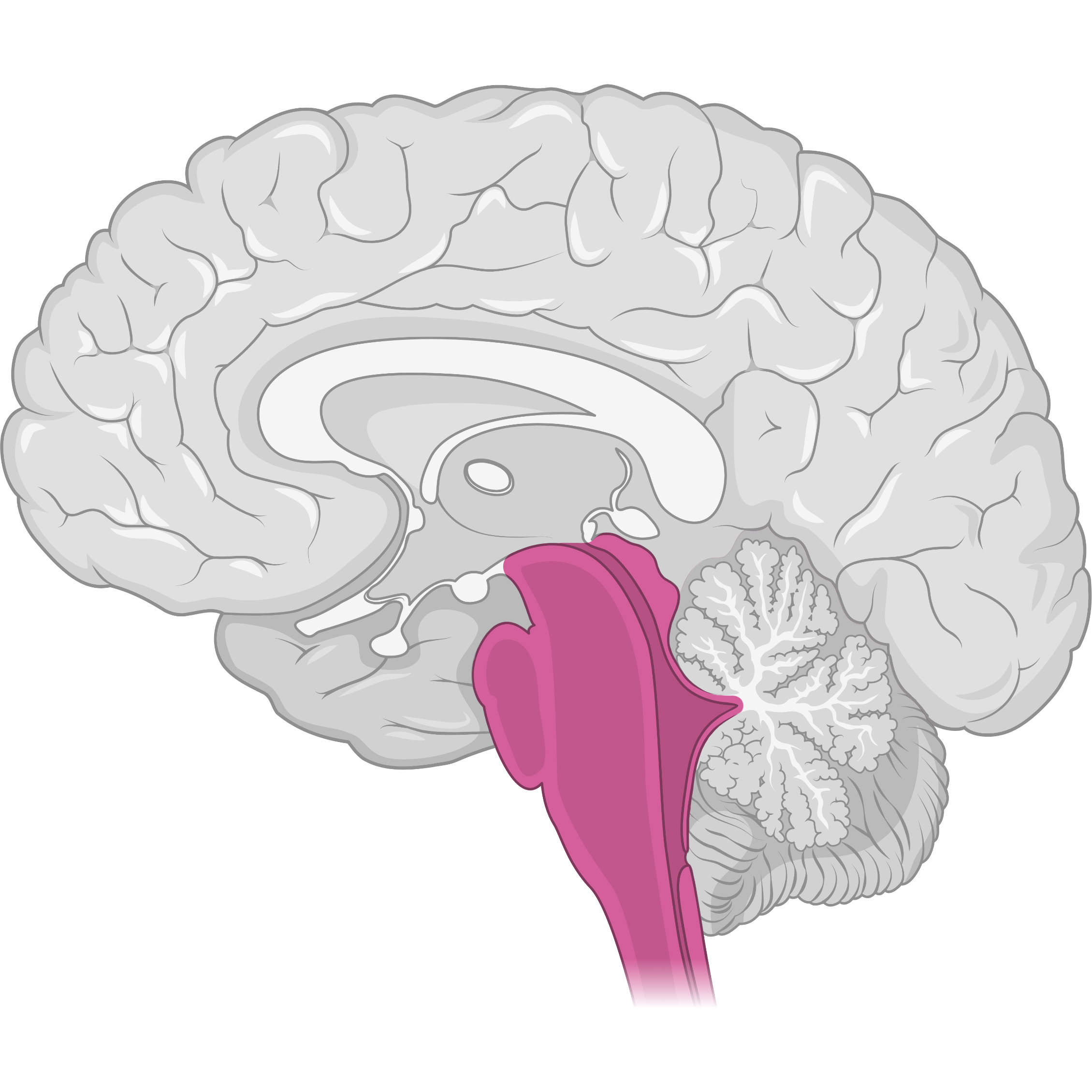
Diffuse Intrinsic Pontine Glioma (DIPG)
20-30 children are diagnosed each year in Canada. DIPGs are located in an area of the brainstem called the pons. DIPG is universally fatal and fewer than 10% of children survive beyond two years from diagnosis.
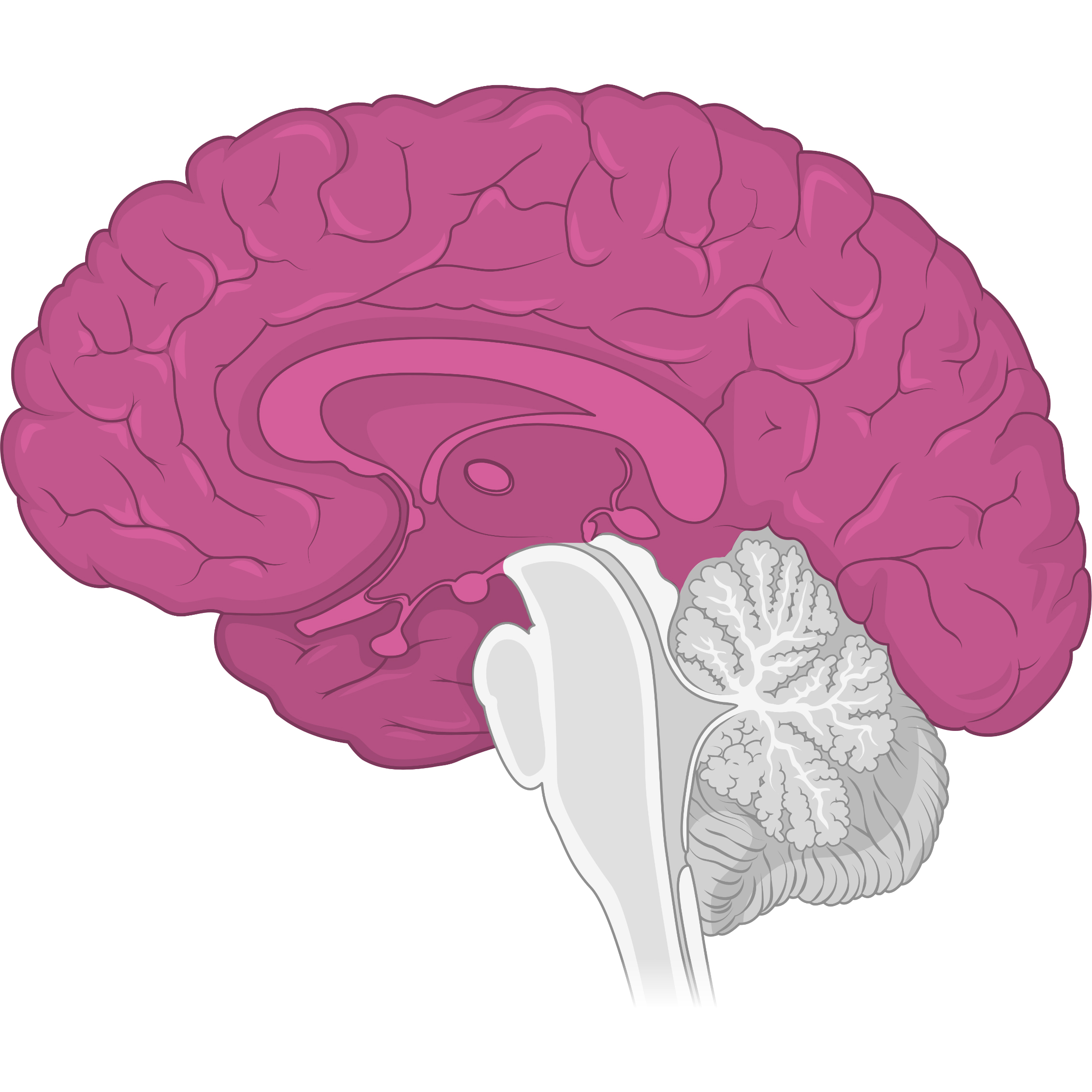
Glioblastoma
4 in every 100,000 people in Canada will be diagnosed with a glioblastoma. These tumours are highly aggressive and typically found in the cerebrum, the largest part of the brain.
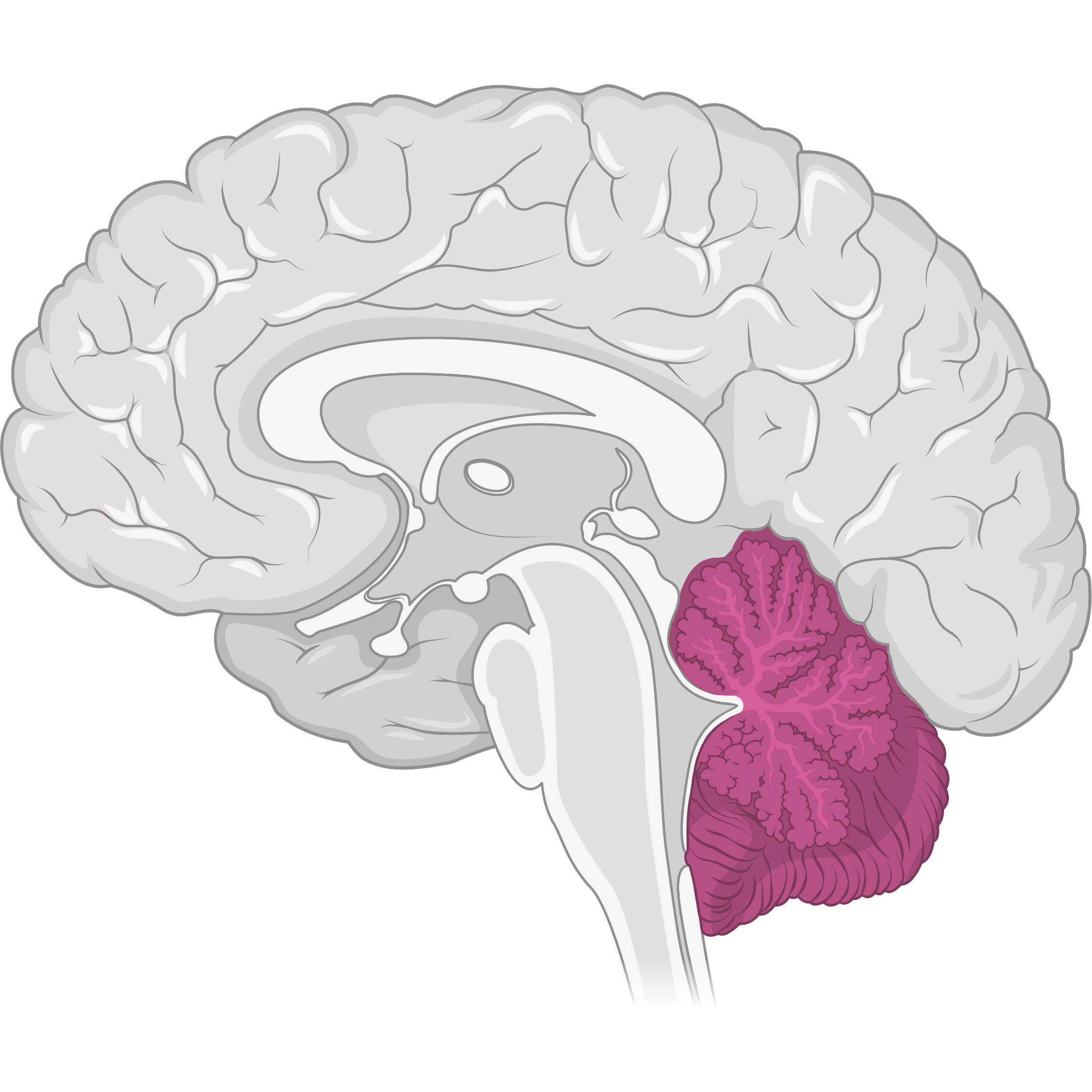
Medulloblastoma
40-50 children are diagnosed each year in Canada. Medulloblastomas are fast-growing tumours that are typically found in the cerebellum, which controls balance and coordination.
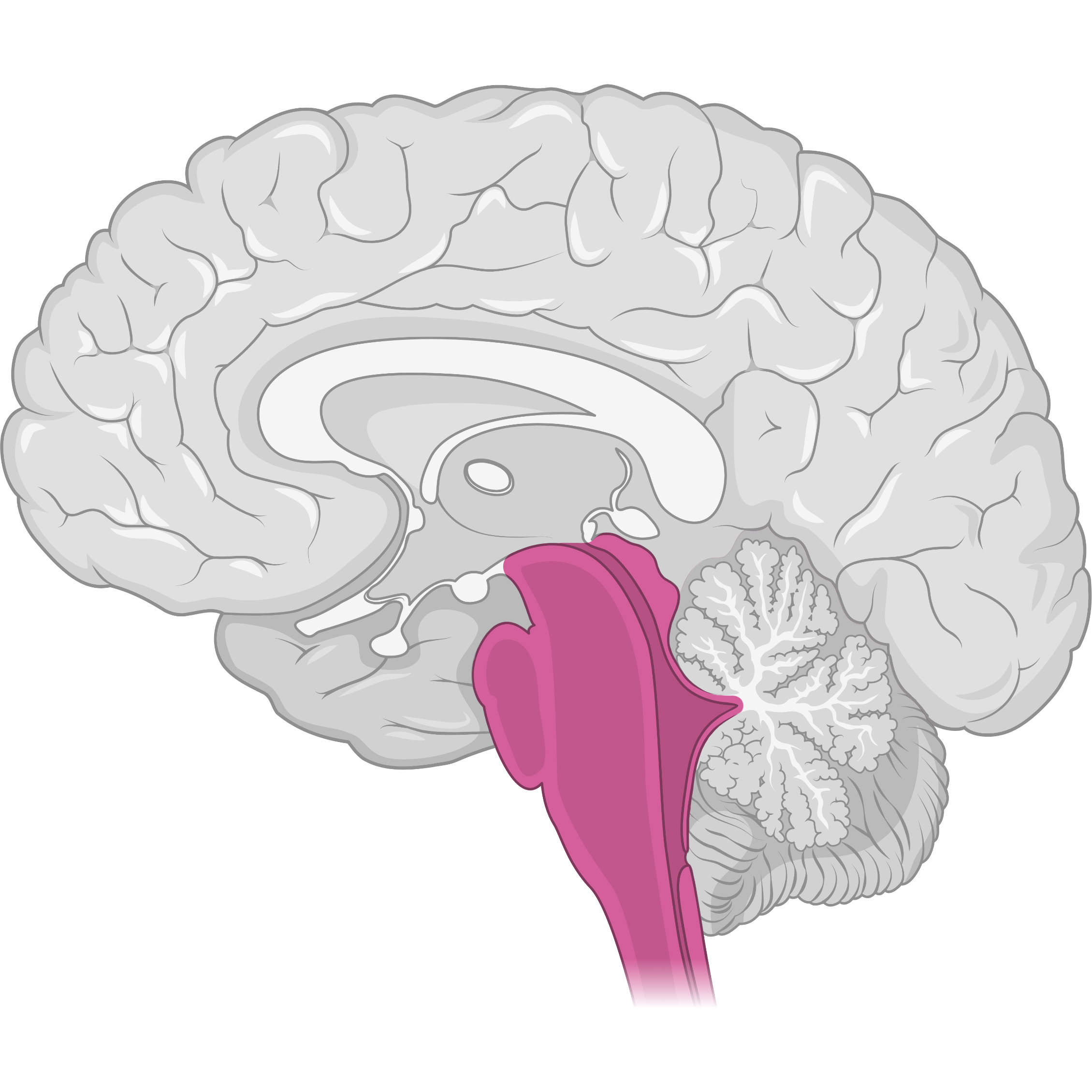
Diffuse Intrinsic Pontine Glioma (DIPG)
20-30 children are diagnosed each year in Canada. DIPGs are located in an area of the brainstem called the pons. DIPG is universally fatal and fewer than 10% of children survive beyond two years from diagnosis.
Tools and Strategies
Our research explores new tools, procedures and strategies to treat these different tumour types. Our current work leverages emerging technologies such as gold nanoparticles and Magnetic Resonance-guided Focused Ultrasound (MRgFUS) enhanced delivery of novel chemotherapies.
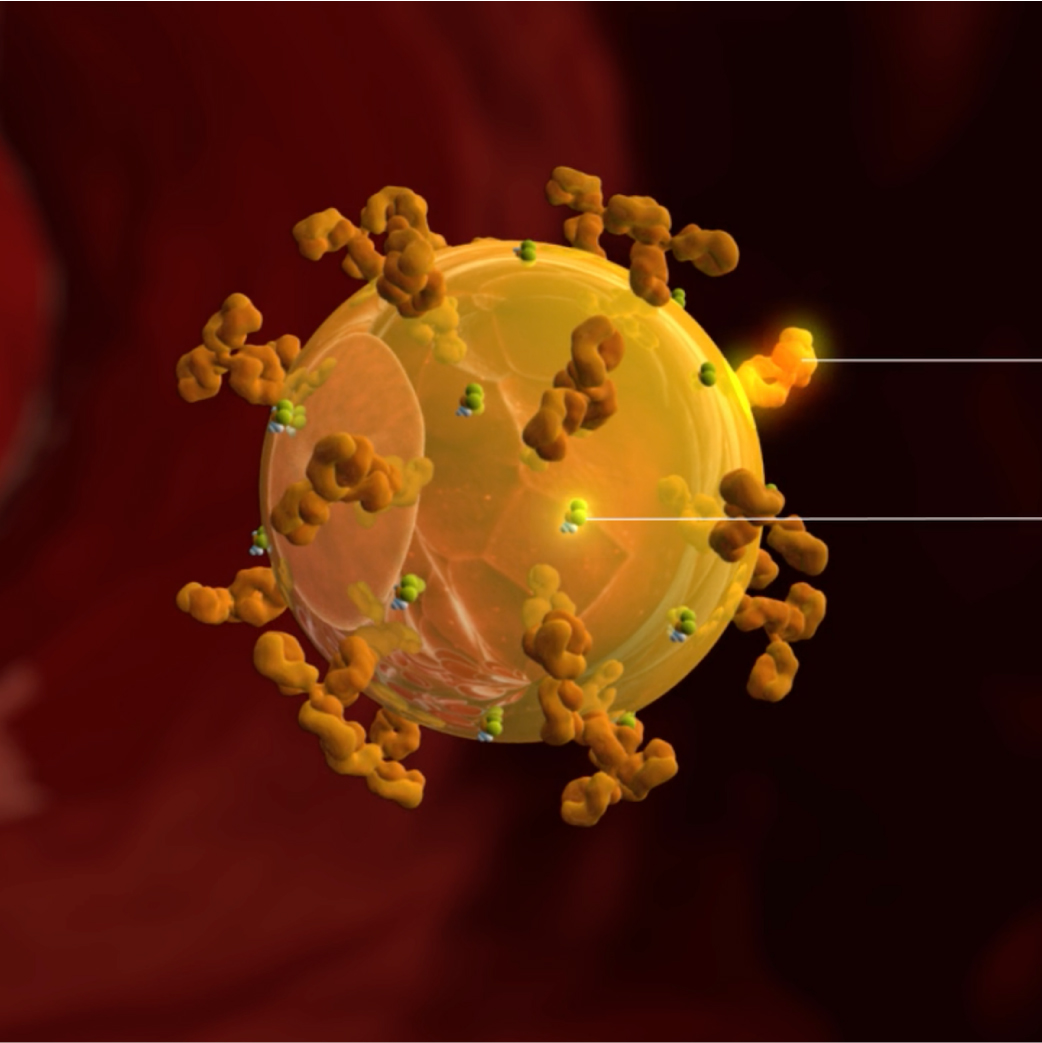
Gold Nanoparticles
Due to their minute size, gold nanoparticles (laden with anti-cancer therapeutics and tumour targeting antibodies) are a valuable tool that can be used to breach the blood-brain barrier.
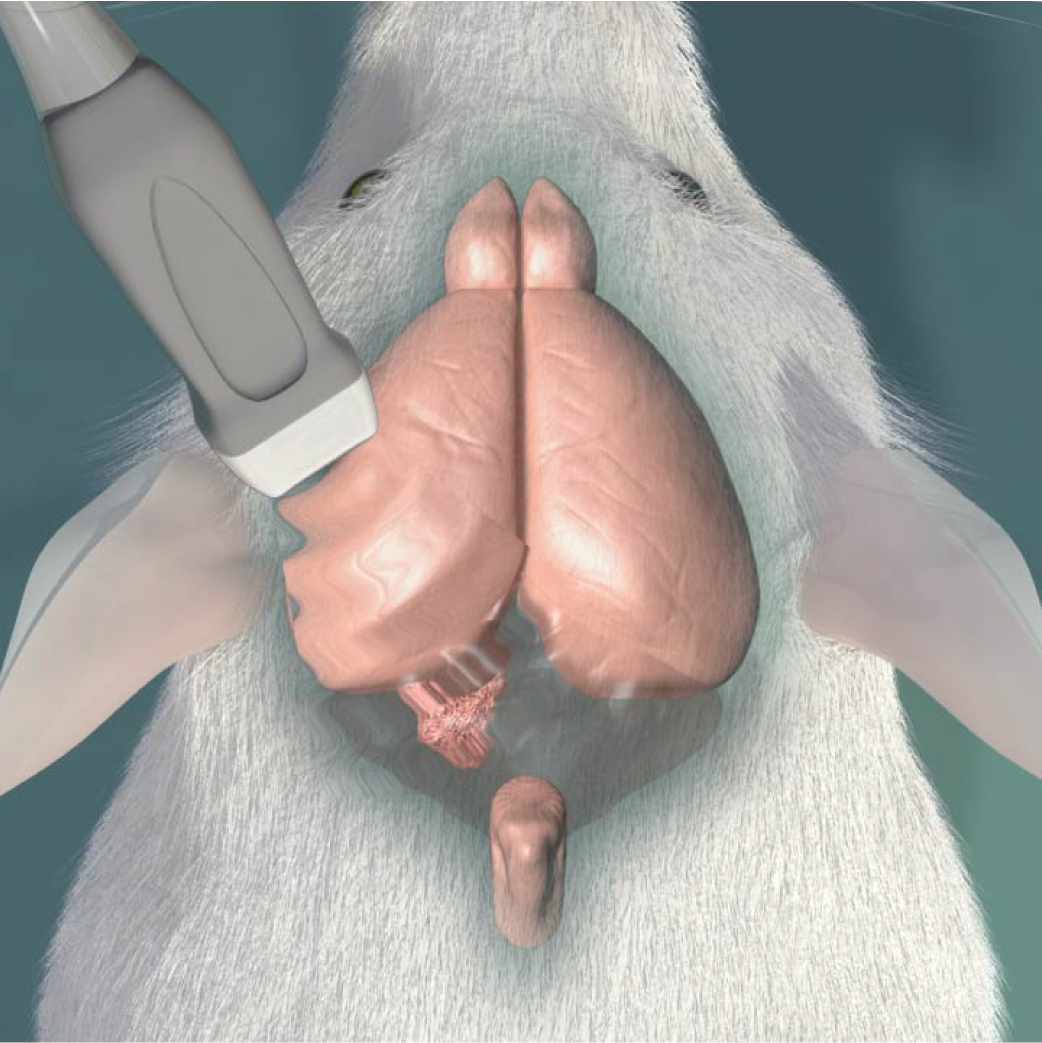
Magnetic Resonance-Guided Focused Ultrasound (MRgFUS)
Safe and gentle ultrasound waves can be directed with precision (using MRI) to tumour locations, temporarily opening the blood brain barrier, allowing therapeutic drugs to reach their tumour targets.
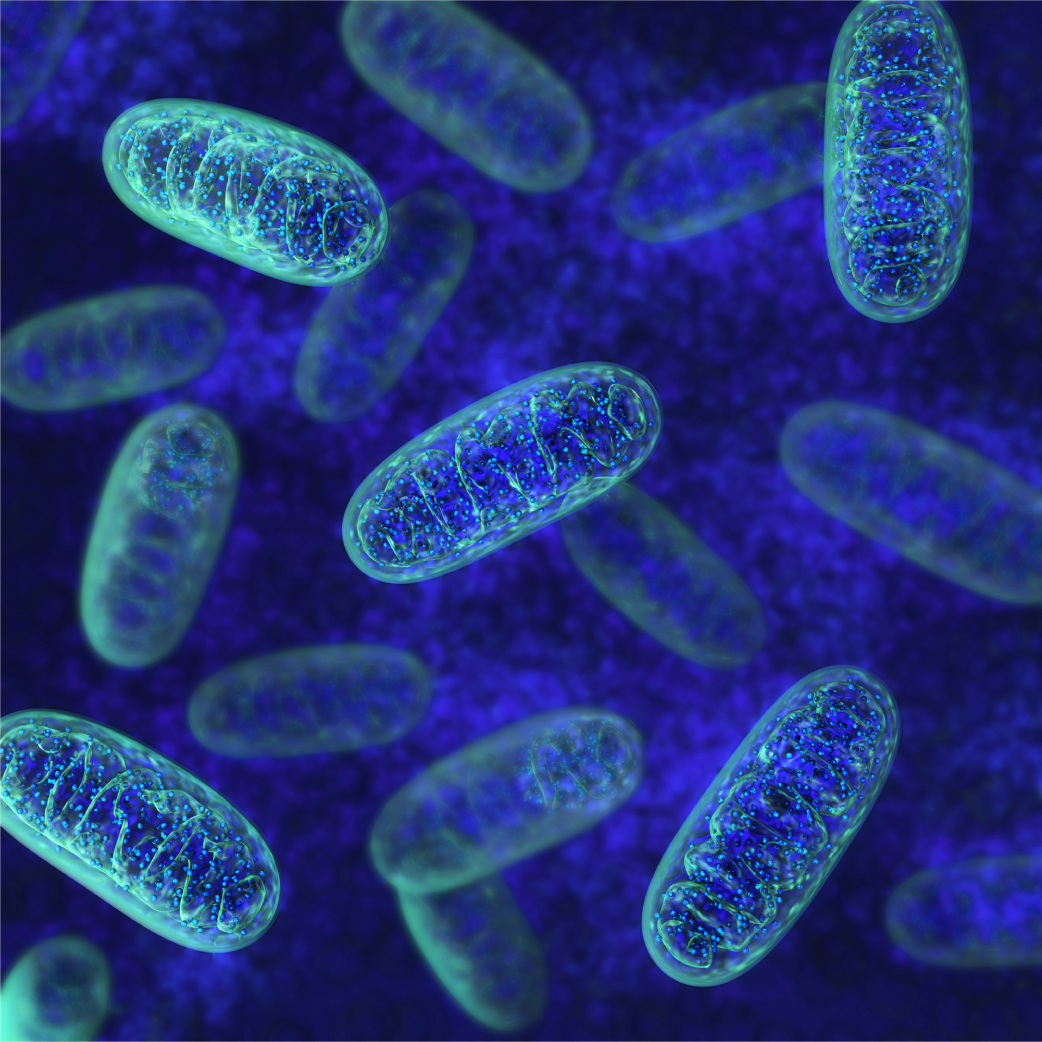
Mitochondria
Mitochondria are responsible for creating the energy that fuels all cells. New research has found that up to 20% of glioblastomas are fuelled by aberrant mitochondrial energetics and may be targetable with drugs.
Gold Nanoparticles
Due to their minute size, gold nanoparticles (laden with anti-cancer therapeutics and tumour targeting antibodies) are a valuable tool that can be used to breach the blood-brain barrier.
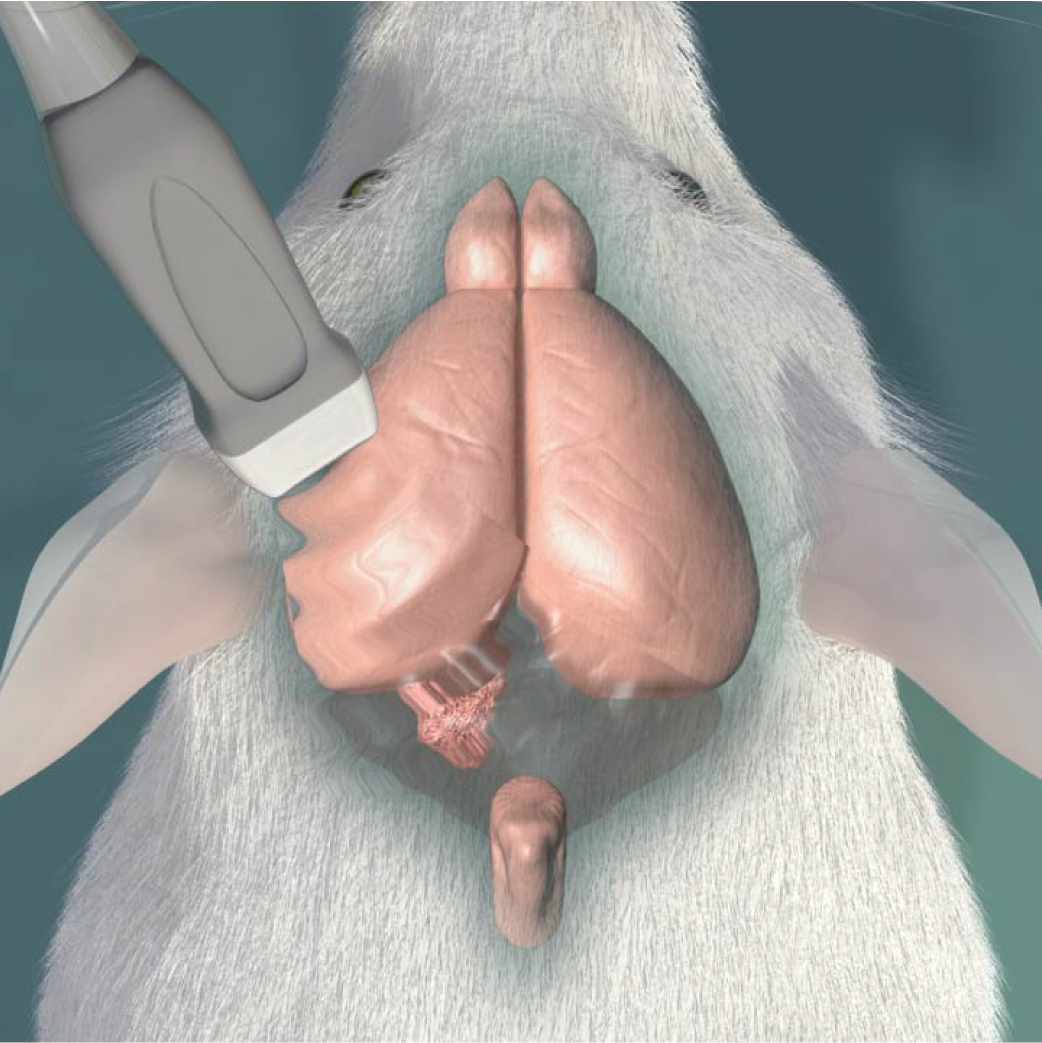
Magnetic Resonance-Guided Focused Ultrasound (MRgFUS)
Safe and gentle ultrasound waves can be directed with precision (using MRI) to tumour locations, temporarily opening the blood brain barrier, allowing therapeutic drugs to reach their tumour targets.
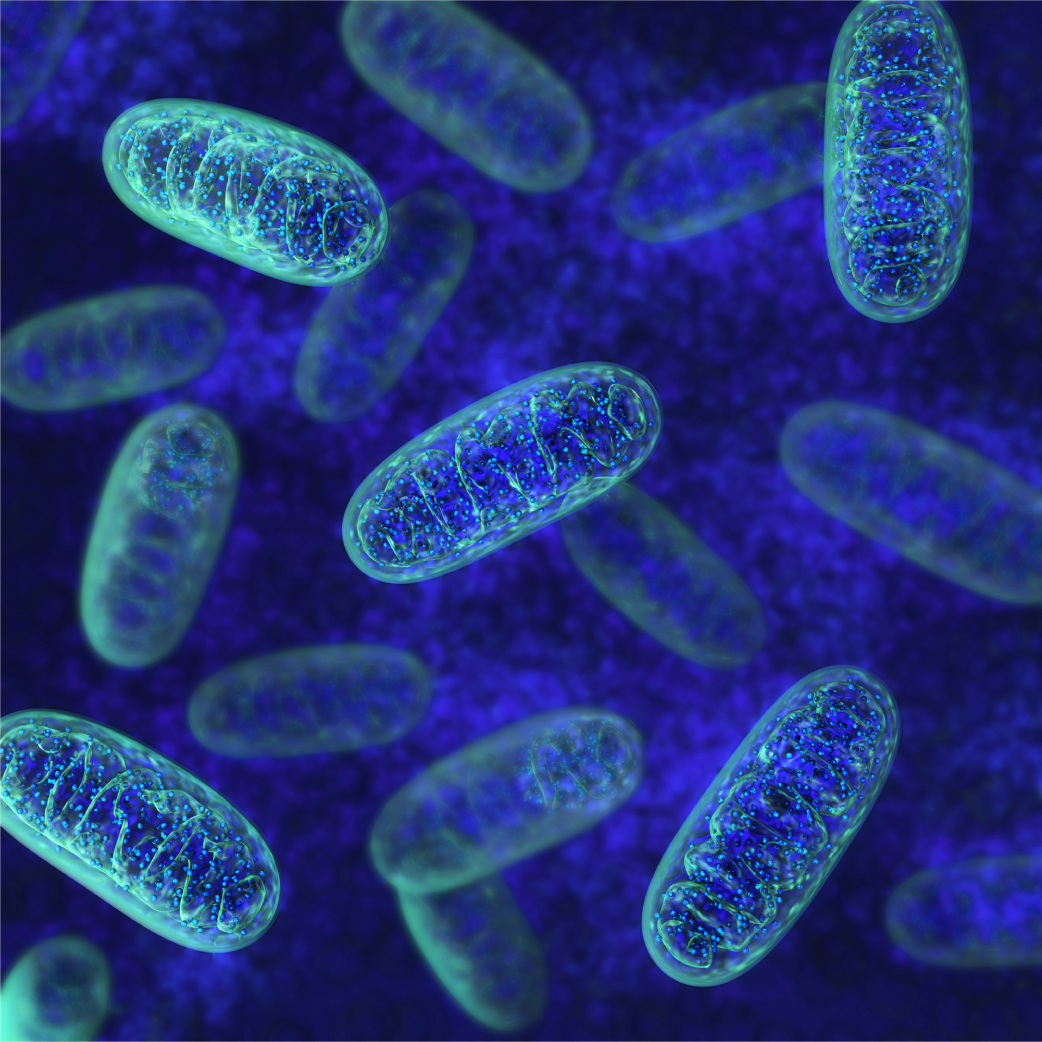
Mitochondria
Mitochondria are responsible for creating the energy that fuels all cells. New research has found that up to 20% of glioblastomas are fuelled by aberrant mitochondrial energetics and may be targetable with drugs.
James T. Rutka
Principal Investigator
The Rutka lab is led by Dr. James Rutka, a paediatric neurosurgeon and Senior Scientist at The Hospital for Sick Children. Dr. Rutka is the former R.S. McLaughlin Professor and Chair of the Department of Surgery in the Faculty of Medicine at the University of Toronto and is the Director of The Arthur and Sonia Labatt Brain Tumour Research Centre (BTRC), one of the largest brain tumour research centres in the world. Dr. Rutka is also the first Canadian to serve as Editor-in-Chief of the Journal of Neurosurgery.
Dr. Rutka began his undergraduate career at Princeton University in Chemical Engineering, then received his MD from Queen’s University followed by a neurosurgery residency at the University of Toronto. He then completed his PhD in Experimental Pathology at the University of California, San Francisco, with a post-doctoral research fellowship in molecular immunology at Juntendo University in Tokyo. He has over 500 peer-reviewed publications and has received numerous awards throughout his career, including the Cushing Medal and the Order of Canada.
James T. Rutka
Principal Investigator
The Rutka lab is led by Dr. James Rutka, a paediatric neurosurgeon and Senior Scientist at The Hospital for Sick Children. Dr. Rutka is the former R.S. McLaughlin Professor and Chair of the Department of Surgery in the Faculty of Medicine at the University of Toronto and is the Director of The Arthur and Sonia Labatt Brain Tumour Research Centre (BTRC), one of the largest brain tumour research centres in the world. Dr. Rutka is also the first Canadian to serve as Editor-in-Chief of the Journal of Neurosurgery.
Dr. Rutka began his undergraduate career at Princeton University in Chemical Engineering, then received his MD from Queen’s University followed by a neurosurgery residency at the University of Toronto. He then completed his PhD in Experimental Pathology at the University of California, San Francisco, with a post-doctoral research fellowship in molecular immunology at Juntendo University in Tokyo. He has over 500 peer-reviewed publications and has received numerous awards throughout his career, including the Cushing Medal and the Order of Canada.
Let’s Get Specific
I want to learn more about…


