Major breakthroughs in the lab
– New discoveries on chronic pain highlighted in Huffington Post
Men and women may process pain differently. Our discovery shows that female and male mice process pain information to the brain differently because the underlying cell types responsible for pain signals are different between the sexes. This paradigm shift, together with the general but massively under appreciated importance of sex differences in medical sciences, means that our discovery will impact the design of future pain research and pharmaceutical drug testing. These findings have far-reaching implications for our basic understanding of pain, how we develop the next generation of medications for chronic pain—which is by far the most prevalent human health condition—and the way we execute basic biomedical research using mice. The implications of the mechanistic sex differences we have discovered are undoubtedly as profound as they are obvious, ranging from diagnostics, to therapeutics, to prevention of chronic pain.
May 26, 2015 – New discoveries on chronic pain highlighted in Eureka Alert
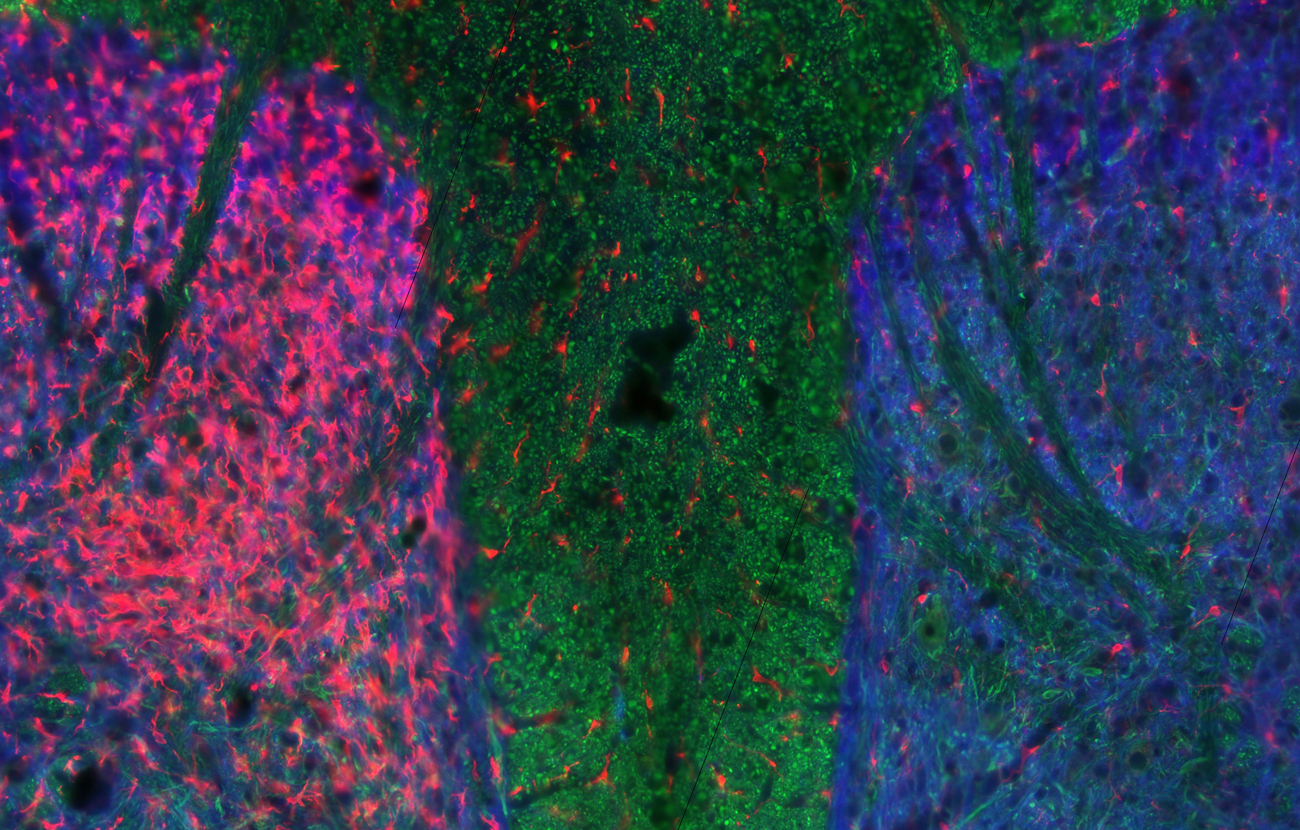
We report an exciting finding elucidating the underlying mechanism behind the hyperalgesic effects of opioid analgesics as used in the treatment of pain. Morphine is the gold-standard for opioid analgesics, however, paradoxically, repeated morphine administration following surgery or injury is known to produce multiple undesired side effects, including increased sensitivity to pain (hyperalgesia), which undermines the analgesic effects. Our findings show that microglia-neuron communication is necessary to produce this effect and in some cases result in increased sensitivity to painful experiences. We anticipate that by targeting the microglia-neuron communication will open the door to new therapeutic strategies for chronic pain.
February 24, 2009 – Learning disabilities breakthrough (CTV News)
A major roadblock in developing new treatments for learning and memory disorders has been in translating fundamental biological knowledge into effective and safe therapeutic approaches. We and our colleagues discovered that a gene called Neto1 is an essential accessory protein of the NMDA (N-methyl-D-aspartate) receptor complex, a critically important protein complex for information storage in the brain. Genetic deficiency of Neto1 has specific and substantial effects on the ability of the NMDA receptor to mediate spatial learning and memory. We found that administration of an ampakine, CX546, at low dose, fully restored spatial learning and memory in mice. This is the first report in the literature of a rescue of an NMDA complex impairment in vertebrates. Consequently, our results formally establish the principle that in vertebrates, an inherited defect in synaptic plasticity and spatial learning can be pharmacologically corrected. This discovery has obvious important implications for the treatment of learning defects and cognitive dysfunctions in humans.
December 14, 2006 – Diabetes breakthrough in Salter lab reported by CBC News
In type 1 diabetes, T cell-mediated death of pancreatic β cells produces insulin deficiency. However, what attracts or restricts broadly autoreactive lymphocyte pools to the pancreas remains unclear. We discovered that a gene called TRPV1, found in pancreatic sensory neurons, controls islet inflammation and insulin resistance. Eliminating these neurons using the neuropeptide substance P delivered by intra-arterial injection into diabetes-prone mice reverses abnormal insulin resistance, insulitis, and diabetes for weeks. Our findings uncover a fundamental role for insulin-responsive TRPV1 sensory neurons in β cell function and diabetes pathoetiology and will bring forth new therapeutic strategies for type 1 diabetes.